Dr. Alexander Weber was my first stop in the journey of all things ACL back home. He works out of USC’s Keck School of Medicine (and my alma mater, go Trojans!) and is a team physician with USC Athletics and the LA Kings. He had operated on my Nextdoor neighbor, and another plus was that he had an opening first thing Monday morning. So bright and early, a friend kindly drove me across town to his office in Glendale.
I was nervous and didn’t totally know what to expect, even though I’d already been seen by two medical clinics. I still harbored hope that the injury wasn’t as severe as originally diagnosed. After hobbling in with the brace and on crutches, and getting through all the standard new patient paperwork and intake, the Dr. walked in and greeted me with an elbow bump. I retold the story of my bad decision making on the mountain, and after more pulling and prodding (Lachman test), he said he did think there was a tear, to which I reacted with a few choice expletives.
He demonstrated the difference between the right and left knee, pulling on both tibias (shins), with more give on my left side. My MCL felt good, so it was most likely just the ACL, but the MRI would also reveal any issues with the meniscus. “What’s a meniscus?” I asked, having opted out of the physiology science class in high school in lieu of biology. “The shock absorber for your knees.” That sounds pretty important, I thought. I was advised to keep with the brace, but the crutches weren’t necessary. I could put weight on the leg, but the first real steps took adjustment as gravity had pulled the swelling down from my knee to my foot.
It was starting to get real, and I told the Dr. that I wanted to get the whole process started and put behind me as quickly as possible, since I had waited a beat with my shoulder dislocation, which made recovery much more dragged out. I was able to get an MRI later the same day, and the Dr. called to relay the findings. “Is it good news?” I asked anxiously, not really knowing how to start the conversation. “Yes,” was the reply. I had a femoral avulsion tear (the ligament is torn off the wall of the bone, see MRI images), and he could most likely perform a repair vs. a reconstruction, but it would be an interoperative decision. I had just finished reading the educational packet given to me at the ski resort clinic, figuring I should start being a good patient, and in the packet it said, and I quote, “The only way to fully fix a torn ACL is with surgery. Doctors rarely sew torn ACLs back together since this most often fails. Instead, doctors replace the ligament with a tendon from another part of the body or from a donor. This is called an ACL reconstruction.”
MRI IMAGES

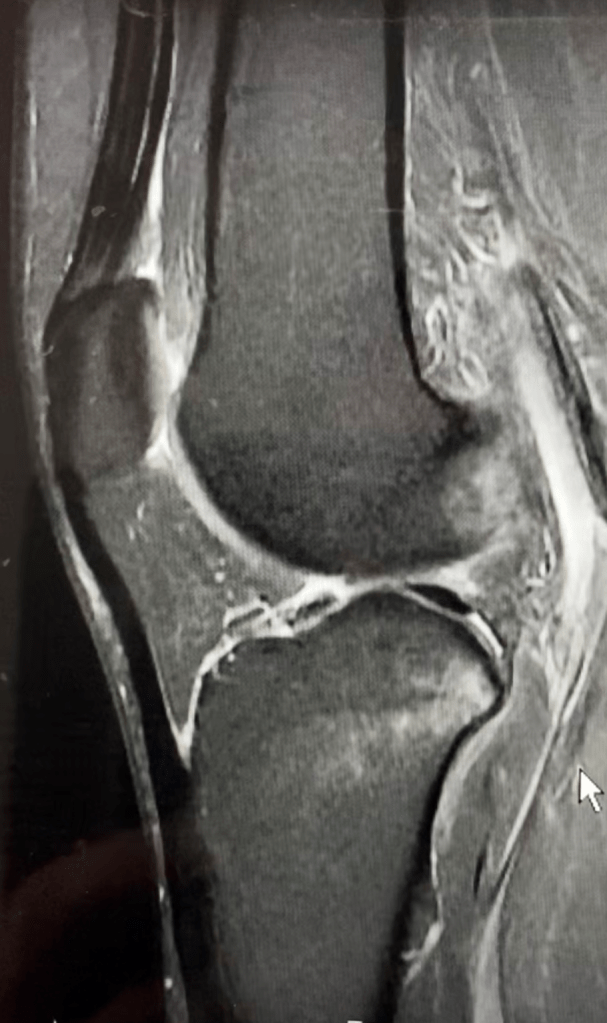

Knowing what I know now, the Dr. was giving me good news, but I didn’t take it that way. “I just read that you can’t repair ACL’s, you have to reconstruct.” I then went into full blown second phase of grief, ANGER, and he did his best to talk me off the ledge. I couldn’t have been the first patient to react the way I did, is what I like to tell myself. The fact that my meniscus was fine didn’t offer much solace. To educate me further, he sent a few medical articles on ACL repair. My main takeaways after getting through the medical jargon were 1) there is drilling involved, 2) repair is not recommended for patients under 21, 3) there are several factors a surgeon will use to assess if repair is possible (tissue quality, location of tear, etc.), but mostly that there is drilling involved. Eek.
With the repair, he was going to put a knee brace (string) in and it would stay there FOREVER. If a reconstruction was required, I would be ok with an allograft (donor ligament), as autografts (patient’s tissue) are recommended for younger patients who are very active, and the rehabilitation process would take 6-9 months. But before surgery and any final decisions were made, I would need to get my knee ready and start prehab – physical therapy 2-3x a week for 2-3 weeks. The goals would be to:
- Reduce swelling
- Regain range of motion
- Regain quad strength
The expectation at the next appointment was that I would walk in like a normal person, no brace, no limp. Observing the overall deer in headlights attitude I had, he advised that I call the recommended physical therapy places to get a sense of their vibe, and decide on one. Scheduling and locations were important as well, as the frequency of visits would be a factor.
VIBE, I can do that, seems simple enough.
CONCLUSION
- While ACL reconstruction is the gold standard, ACL repair is possible, but it’s an interoperative decision made by your surgeon (more on repairs in a later post)
- Surgery does not always happen immediately after the accident, swelling needs to go down and quad strength regained, as you will lose quad strength post-operation
- Especially if you live in a large city with many options for healthcare professionals, go with their vibe and your gut. It is a big decision, it is your body, and a long recovery journey. You need to feel comfortable with everyone that’s part of your healthcare team. DO NOT FEEL PRESSURED INTO ANYTHING YOU DO NOT WANT TO DO. While Top Doctor lists are great, I err on the side of personal testimonials, especially those with recent experiences to best gauge
- Be clear with your doctor about expectations and your lifestyle. The clearer you are, the better it ensures everyone is aligned and equipped to set you up for success. Surgery is not required with an ACL tear, but there are higher probabilities of long term damage if you go back to an active lifestyle
- Physical Therapy = LOCATION, LOCATION, LOCATION. I got a little starstruck in researching where pro-athletes get treated, but picking a rehab center in your area is important as it’s a weekly commitment. There is more give with the Dr. as those appointments are more spread out
- I did get a 2nd opinion elsewhere but decided to stay with Dr. Weber. The other Dr. was incredibly nice and also highly recommended, but perhaps since I was still so emotional, his vibe was a little more casual than what I needed
- There are several donor sites for autografts: patellar, hamstring, or quad. I’m seeing that quad is becoming a popular choice among sports orthopedics, as there can be residual knee pain. Ask your Dr. for their recommendation/what they feel comfortable with


One response to “Official Diagnosis”
[…] huge milestone in ACL rehab (see my ACL accident post here) is running, and they start you on an anti-gravity treadmill. The first day I was at 50% weight and […]
LikeLike